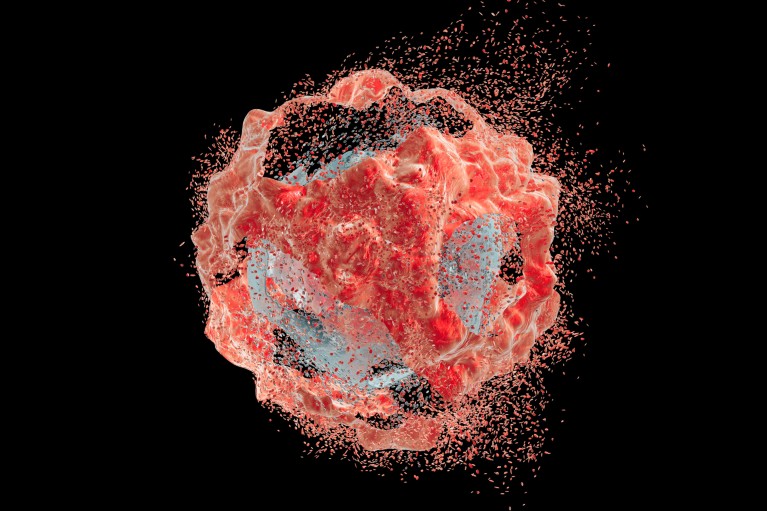
Targeting exposed CLDN1 on tumours could help kill cancer cells and break down the collagen barrier, improving access for immune cells and immunotherapies.Credit: Kateryna Kon/Science Photo Library/Getty Images
Claudin-1 (CLDN1) is a protein usually found nestled between epithelial cells — which cover internal and external body surfaces — helping to bind them. “It works like a zipper to keep two cells together,” says Luigi Manenti, chief medical officer at Alentis Therapeutics, a biotechnology company headquartered in Basel, Switzerland.
In many solid tumours, CLDN1 is overexpressed and can drive remodelling of the extracellular matrix, forming a dense collagen barrier around the growth.
“This barrier helps shield the tumour from the immune system and immunotherapies, leading to poorer outcomes for patients,” says Josep Tabernero, head of medical oncology at the Vall d’Hebron University Hospital, Barcelona.
After a decade of research, Alentis’s founder, Thomas Baumert, developed the first antibody that binds only to the exposed form of CLDN1 expressed in the disease1, laying the foundation for a growing pipeline of anti-CLDN1 antibodies and antibody-drug conjugates (ADCs). Oncology programmes include ADCs ALE.P02 and ALE.P03, which are progressing towards clinical trials. Most advanced is ALE.C04, a first-in-class therapeutic antibody designed to specifically target exposed CLDN1 on tumour cells. Upon binding, it orchestrates cancer-cell death through antibody-dependent cell-mediated cytotoxicity, as well as facilitating the breakdown of the collagen barrier, improving access for immune cells and immunotherapies.
Unmet clinical need
Among the 27 known members of the claudin family, CLDN1 stands out for its role in the development and progression of several different cancer types2, including head and neck squamous cell carcinoma (HNSCC).
“CLDN1 overexpression is almost universal in patients with advanced HNSCC,” says Tabernero. “And around 30% of these tumours express very high levels of this protein.”
HNSCC is the seventh most common cancer globally, with around 890,000 new cases and 450,000 deaths annually3. In its advanced stages, there are very few treatment options.
“We presented a package of preclinical and translational data showcasing ALE.C04’s efficacy against CLDN1-positive tumours, both alone and in combination with an existing immunotherapy treatment,” says Manenti. “Based on these results, we were given the green light to advance into a clinical trial.”
A phase I/II study is now underway (NCT06054477) to evaluate the safety and efficacy of ALE.C04 — both as a monotherapy and in combination with the immunotherapy pembrolizumab — in patients with advanced HNSCC.
In 2023, the US Food and Drug Administration granted Fast Track designation to ALE.C04 for the treatment of patients with recurrent or metastatic CLDN1-positive HNSCC.
Standing out from the crowd
Several pharma firms have focused on targeting other members of the claudin family, including CLDN18.2 for the treatment of gastrointestinal cancers4. But Alentis is committed to exploring the untapped potential of CLDN1. Outside of oncology, the company has developed a first-in-class antibody, lixudebart (formerly known as ALE.F02), for liver (NCT05939947), kidney (NCT06047171) and lung fibrosis, which is designed to block fibrotic signalling and break down the collagen barrier to preserve organ function.
“The overexpression of CLDN1 in cancer gives us an opportunity to harness this potential using an array of therapeutic modalities, including ADCs,” says Manenti.
“We know that many other solid tumour types also overexpress CLDN1, including cholangiocarcinoma (bile duct), squamous-cell lung cancer and colorectal cancer,” says Tabernero. “Therapeutic opportunities for CLDN1-targeted therapies could extend to many more cancer patients, both as a monotherapy or in combination with standard of care.”


